Current projects led by Robert A. Kloner, MD, PhD, include studies designed to reduce the amount of damage that occurs during experimental myocardial infarction (heart attack). In the United States, there are more than 800,000 heart attacks per year, and this remains a major cause of morbidity and mortality. One month mortality can be as high as 10%, and nearly a quarter of older people suffering heart attack develop heart failure.
Limiting the number of cells that die after coronary artery occlusion is one way of reducing mortality and morbidity after a heart attack; this approach remains a major focus of the laboratory. The laboratory has had success with some treatments: preconditioning, hypothermia, pharmacologic therapies such as mitochondrial protective proteins, a delta opioid antagonist, and others. Researchers are currently exploring the effect of antidiabetic drugs called SGLT-2 inhibitors on heart attack size. Other studies have also explored therapies to prevent or treat heart failure and left ventricular dilatation after a heart attack.
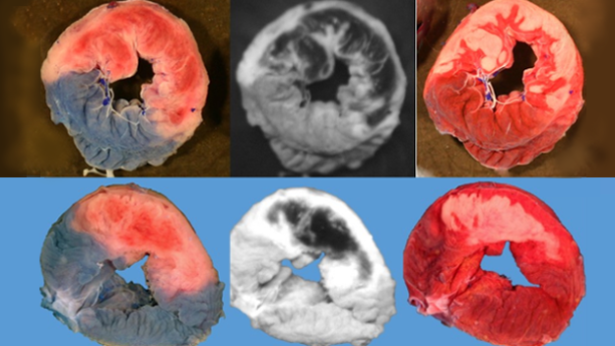
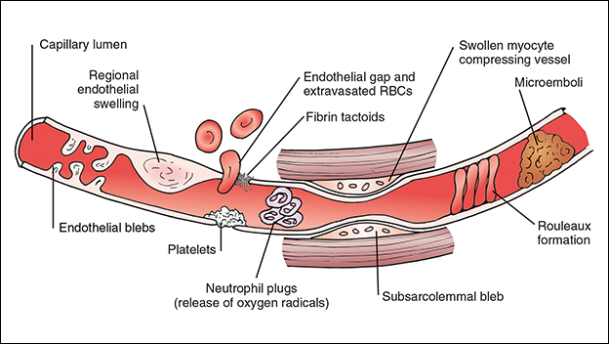
The no-reflow phenomenon refers to the inability to perfuse the microvasculature after re-opening the large occluded epicardial coronary artery, which is the primary cause of a heart attack (Fig. 1, 2). Researchers have studied the no-reflow phenomenon and its effect on adverse left ventricular remodeling following a heart attack and have also been working on therapies to reduce this devastating consequence of a heart attack. The laboratory is exploring several therapies for the no-reflow phenomenon. SGLT-2 inhibitors appear promising.
Fig. 1: What does the ischemic risk zone, no-reflow and myocardial infarct (heart attack) look like? Representative sections taken as transverse sections through the left ventricle of two experimental models ( row top and bottom) showing risk zone (left, area without blue pigment staining), zone of no-reflow (middle, dark, non-fluorescent areas show where blood failed to penetrate during reperfusion), and necrosis (right, brick red represents viable myocardial tissue and the pale white area is the necrotic tissue; that is the myocardial infarction or heart attack).
Fig. 2: Causes of the no-reflow that inhibits blood flow in small blood vessels in the wall of the heart after proximal coronary artery occlusions are removed.
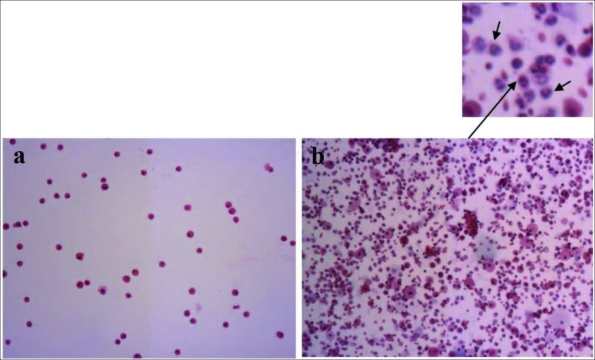
Fig. 3: One acute exposure to e-cigarette smoke associated with inflammatory cells taken from the lung.
The laboratory has also been involved in cardio-toxicology studies, exploring the effects that electronic cigarettes (vaping) have on heart and lung function and pathology, showing infiltration of inflammatory cells into the lungs after vaping (Fig. 3). These studies, carried out with our collaborators at the University of California Irvine (UCI), have suggested that e-cigarettes may not be as safe as initially thought and may have adverse effects on the heart and lungs. Recent studies have found that exposure to e-cigarettes with nicotine impairs the ability of blood vessels to dilate normally and may suppress the immune response of the heart.
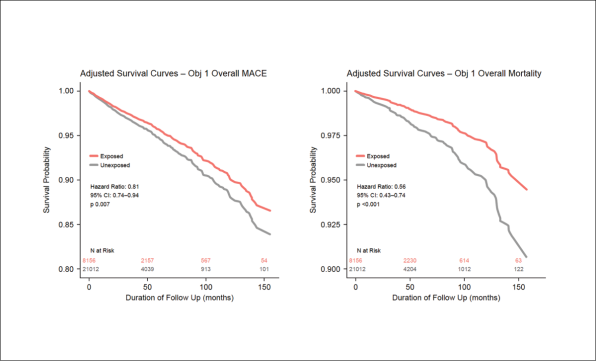
Fig. 4: Exposed = Exposed to tadalafil (PDE-5 inhibitor); Unexposed = not exposed to tadalafil. MACE = major adverse cardiovascular events. These survival curves show that patients with erectile dysfunction who receive tadalafil (Cialis; orange lines) had better survival free of MACE and better overall survival than those not exposed (controls; grey lines).
Dr. Kloner is involved in epidemiological studies exploring the effect of the class of drugs called phosphodiesterase-5 (PDE-5) inhibitors on cardiovascular outcomes in men being treated with these drugs for erectile dysfunction. Recent studies from their research group have suggested that this class of drugs may have cardioprotective effects and is associated with lower rates of adverse major cardiac events in a population of men taking these drugs (Fig. 4). These drugs were also associated with a lower rate of overall mortality and cardiovascular mortality. A current study is analyzing the results of a long-acting phosphodiesterase-5 inhibitor on cardiovascular outcomes.
In collaboration with Dr. Niema Pahlevan in the engineering department of the University of Southern California and James Boswell Postdoctoral Fellow Dr. Rashid Alavi, Dr. Kloner’s group is exploring novel, noninvasive ways of assessing heart function and diagnosing coronary artery occlusion by mathematical analysis of the carotid artery waveform shape and machine learning. The shape of this waveform can be assessed by a cell phone application, and was shown to predict reduced left ventricular function in heart failure patients with 90% accuracy.
In collaboration with Dr. Xianghong Arakaki and the HMRI neuroscience group, Dr. Kloner and collaborators at UCI are studying the effect of heart rate variability and its relationship to early signs of dementia, such as Alzheimer’s disease and its correlation to other neurologic abnormalities, including the volume of certain regions of the brain, Neuro-psychological abnormalities, and EEG findings.
HMRI conducted a foundation-funded study with Los Angeles County, the University of California Los Angeles, and other institutions to examine the effects of COVID-19 on emergency surges and increases in out-of-hospital cardiac arrests. Research suggests that the healthcare system in LA County successfully minimized the time to treat heart attacks, which was not really affected by COVID-19; this is a positive statement about the LA County Healthcare System. Additionally, the increase in cardiac arrest during the pandemic was due to those affected avoiding the hospital instead of seeking emergency life-saving care.
Over the last year, the laboratory has been developing an experimental model of stroke. Stroke affects nearly 800,000 people in the US per year, accounts for one in 5 deaths, and results in disability in about half of patients. Drs. Dai and Kloner are working on new therapies that appear promising in reducing the size of strokes and will be presenting some of this data for the first time at the annual American Heart Association Scientific Sessions in Chicago in November 2024.