HMRI’s History of Impact
Legacy of Scientific Innovation
HMRI’s legendary scientific discoveries date back to the 1950s with the establishment of two research facilities: Pasadena Foundation for Medical Research (PFMR), founded by Dr. George Sharp in 1952, and the Institute of Medical Research of Huntington Memorial Hospital (which also housed the Pasadena Neurovascular Foundation), founded by Dr. C. Hunter Shelden in 1953. A past rooted in growth and mergers, innovative technologies, scientific breakthroughs, and life-changing discoveries that improve human health has built the HMRI of today — a leading, world-class biomedical research organization.

CSF Shunt System
Robert H. Pudenz, MD, developed the cerebrospinal fluid (CSF) shunt system for hydrocephalus, also known as “water on the brain.” This neurological disorder occurs when an excessive amount of CSF accumulates within the ventricular cavities of the brain, resulting in rapid enlargement of the head. The Pudenz valve system is still commonly used today. According to the Hydrocephalus Foundation, hydrocephalus affects more than one million Americans, and over 36,000 shunt surgeries are performed every year.
Educating the Next Generation
HMRI’s legacy of educating future generations of scientists in 1955, shortly after its founding, when the research institutes began attracting talented postdoctoral researchers to work alongside its pioneering scientists and physicians.
Automobile Safety and Seatbelts
Dr. C. Hunter Shelden's research and treatment of head injuries resulting from automobile accidents led to important safety features that have saved millions of lives – retractable seatbelts, recessed steering wheels, reinforced roofs, roll bars, door locks, seatbacks, and airbags. In 1959, Congress passed groundbreaking legislation requiring all automobiles to meet the safety standards recommended by Dr. Sheldon.
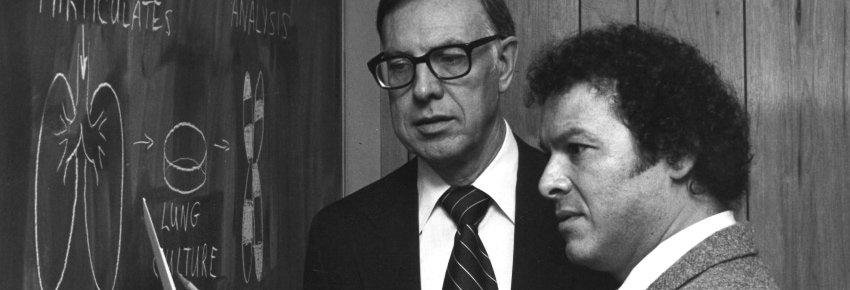
Lung Cancer and Smog
A collaboration between Dr. Donald E. Rounds and Dr. C.M. Pomerat of the Pasadena Foundation for Medical Research resulted in the first scientific evidence that human lung cells exposed to smog undergo changes characteristic of the early stages of cancer. Their work provided evidence to support the hypothesis that smog can cause lung cancer. “The experiments show there are sufficient carcinogens in the atmosphere to trigger the initial steps toward malignancy,” said Rounds.
Every year, more people die of lung cancer than prostate, breast, and colon cancers combined. The pioneering research at HMRI Their research provided the critical link between smog and lung cancer, and a catalyst for smog regulations to improve air quality and reduce the incidence of smog-related lung cancer diagnoses.
HIAMR
In 1967, the Institute of Medical Research became the Huntington Institute of Applied Medical Research (HIAMR).
Cardiovascular Research Commences
In 1969, Dr. Richard Bing, known as the “Father of Cardiac Metabolism,” joined HIAMR and served as the director of Experimental Cardiology. His major contributions include the introduction of high-speed cinematography to view the microcirculation of the heart, a technique to study blood vessel function using nitric oxide, and the use of endothelial cells to study mechanisms, such as endothelium-derived relaxing factor (EDRF), to relax the blood vessels.
Cardiovascular diseases continue to be the leading cause of death worldwide. The World Health Organization attributes 17.9 million deaths to cardiovascular disease each year. At HMRI, cardiovascular researchers remain committed to research and cutting-edge discoveries that reduce the size and severity of heart attacks and stroke.
Lasers to Surgically Remove Tumors
Starting in 1963 and continuing into the 1970s, HMRI began experimenting with laser beams for use in the surgical removal of tumors. Don Rounds understood that it wasn’t being able to burn things up that mattered but that the laser energy could be medically useful at lower intensities. Since then, the medical community has found myriad uses for laser technology, including shrinking or destroying tumors, preventing blood loss by sealing small blood vessels, refractive eye surgery, dental procedures, dermatological treatments, and more.

Immortal PC3 Cell Line Dr. Lawrence W. Jones worked with other scientists in the institute’s Cell Culture Laboratory to conduct early research on prostate cancer cells. They were among the first teams to identify organ-specific markers in human epithelial cells in single cell culture. Researchers successfully grew immortalized lines of tumor cells originating in human prostate cancer, including the immortal PC3 human prostate cancer cell line. These cells are now widely used to test new, life-saving prostate cancer drugs, assess their response to chemotherapy, and study biochemical changes in advanced prostate cancer cells.
Huntington Medical Research Institutes (HMRI)
The modern era begins. The El Molino (PFMR) and Fairmount (HIAMR) operations merged in 1982 and gave birth to the modern era of Huntington Medical Research Institutes (HMRI) as it is known today.

MRI for Medical Imaging
During this era, HMRI researchers pioneered the use of powerful magnets in medicine, the precursor to magnetic resonance imaging (MRI), in 1983. They conducted comparative studies of computer tomography versus MRI, contributing to the regulatory approval of magnetic resonance for medical imaging. HMRI’s role was to recognize and demonstrate how MRI had actual value in medical practice. The advisory team we developed was part of the program’s strength, including leaders from Oxford, Bell Labs, Caltech, Harvard, and UCSF.
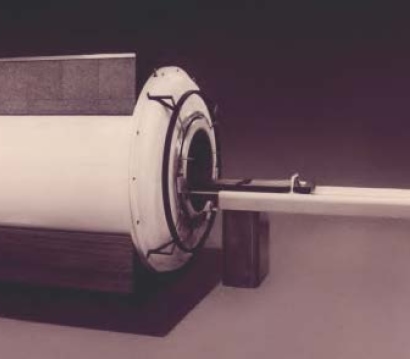
Brian D. Ross, MD, director of HMRI’s Magnetic Resonance (MR) Laboratory, trained many postdoctoral fellows in magnetic resonance spectroscopy (MRS), which employs MR technology to detect tissue chemistry. He developed an important technique for MRS analysis of the brain, and his lab demonstrated MRS’s value as a sensitive diagnostic tool for brain tumors, dementia, stroke, encephalopathy, head trauma, epilepsy, and more. At HMRI, the first 1000 professional radiologists were trained in MRI, and the first 300 specialists were trained in MR Spectroscopy. An estimated 50,000 MRI systems are now installed globally, and over 95 million scans are performed worldwide every year.
Leading the way in Neural Engineering
In 1990, Prentice Hall published Neural Prostheses: Fundamental Studies, edited by HMRI's William Agnew, PhD and Douglas McCreery, PhD. The book reviewed the subject of neural stimulation from the perspectives of safety and efficacy. HMRI’s researchers led the way in the field of neural engineering, developing and testing systems for electrical stimulation of the brain and nerves. Physicist Leo A. Bullara invented the Huntington helix electrode, which has been implanted on the vagal nerves to effectively connect to nerves and the brain to signal patterns for use in deafness, bladder control, and epilepsy.

Alzheimer’s Disease and Brain Aging
The original Brain Again Study at HMRI began in 2000 and was supported by funding from a few family foundations. Researchers aimed to detect protein changes in Alzheimer’s disease (AD) by analyzing 100 cerebrospinal fluid (CSF) samples in people with and without AD, using 2D-gel electrophoresis.

Findings showed inflammatory changes associated with lipids in CSF. This attracted the attention of Dr. Alfred Fonteh, who was using state-of-the-art technology to characterize lipids critical to human diseases at Wake Forest University School of Medicine, where he was a Research Associate and Professor of Internal Medicine. He contacted HMRI’s researchers to request CSF samples so he could conduct advanced chemistry analysis using Gas Chromatography/Mass Spectrometry (GC/MS). Dr. Fonteh’s results were promising – showing changes in lipids and enzyme activity in AD. His interest in the Institute’s clinical studies grew, and in 2001, he joined the HMRI research team.
Liver Research Begins The HMRI Liver Center opened its doors in 2005. HMRI perfected medical resonance spectroscopy that serves as a particularly sensitive diagnostic tool for brain tumors, dementia, stroke, encephalopathy, head trauma, infections, cancers, pediatric hypoxia, multiple sclerosis, epilepsy, and cardiovascular conditions.
Brain Aging Study Evolves
In 2011, the trajectory of the Brain Aging Study changed when researchers received a sizable grant from a private foundation for neuroscience and imaging. This additional funding was transformative in the study’s evolution. The study changed from cross-sectional to longitudinal, enabling scientists to follow the same people over time and observe changes in their brains related to aging; in fact, 227 of the original participants in the longitudinal study are still active participants today. New equipment was purchased for analysis, including a high-tech LC/MS in 2023 to include the measurement and role of omega 3/6 fatty acids. This also supported research for noninvasive biomarkers.
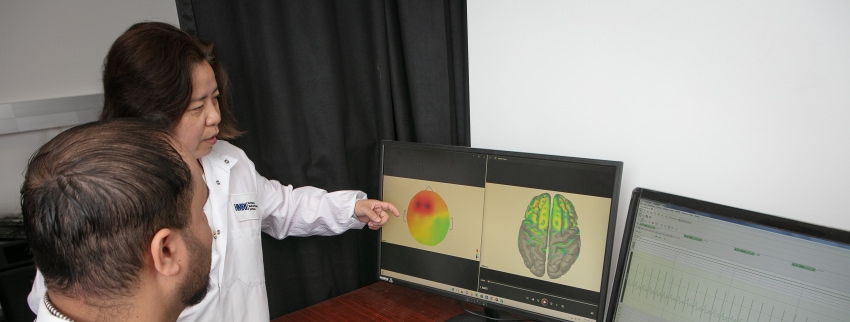
In 2015, electroencephalogram (EEG) analysis was added to the Brain Aging Study projects. Neuroscientist Dr. Xianghong Arakaki was studying migraine and traumatic brain injuries.
She expanded her EEG studies to the aging cohort. Her research showed similar changes in brain wave measurements in cognitively healthy individuals with a high risk of cognitive decline, compared to those with low risk. This led to Dr. Arakaki’s studies on heart waves and heart rate variability to understand the vital connection between the heart and the brain.

State-of-the-art Research Facility
HMRI completed the construction of its new building at 686 South Fair Oaks Avenue in 2018, with generous support from individual donors. Staff moved from two separate Pasadena locations at Fairmont Avenue and El Molino Avenue to the current state-of-the-art laboratory facility, which helped usher in a new era of collaboration among scientists.
Heart-Brain Connection
HMRI appointed Robert A. Kloner, MD, PhD, as the institutes’ chief science officer and director of cardiovascular research in 2018. His leadership directed HMRI’s research agenda, emphasizing cardiovascular disease, neurosciences, and the vital connection between the heart and brain.
Dr. Kloner has made major contributions to the understanding and treatment of heart disease. He performed some of the first studies on and helped define the concepts of no reflow in the heart, stunned myocardium, remote ischemic preconditioning, and triggers of cardiovascular events. He has made significant contributions to the understanding of pathophysiology of heart attack, treatments for heart attack; studies on high blood pressure and heart failure; the effect of toxins like alcohol, cocaine, electronic cigarettes and pollution on the heart; stem cell therapy for the heart; and the intersection between sexual dysfunction and cardiovascular disease. Dr. Kloner is also collaborating with a bio-engineering group (cell phone app) at USC for noninvasive assessment of heart function.

Advances in Neuropsychiatric Diseases
In 2020, Dr. Anju Vasudevan, Chair of Basic and Translational Neurosciences and founder of the Angiogenesis Brain Development Laboratory (ABDL) moved her lab from Harvard to HMRI. While on the faculty at Harvard, she discovered a paradigm-shifting framework to address the urgent global mental health crisis.
Traditionally, research on neuropsychiatric conditions has been neurocentric, focused on treating the neurons and brain cells. Her research took a new approach by investigating blood vessel formation (angiogenesis) in the developing embryonic brain and its impact on adult behaviors. Disruptions in prenatal or postnatal brain development can lead to neuropsychiatric diseases, including epilepsy, autism, schizophrenia, anxiety, and depression.
Dr. Vasudevan investigates these key events of brain development and how those can go wrong. Her long-term goal is to ensure that brain development remains on track.
Intracellular Signaling Advances the Heart-Brain Connection
HMRI deepens its understanding of the connection between the heart and brain by investigating molecular pathways. Nicole H. Purcell, PhD, professor of cardiovascular research, joined HMRI in 2021 to lead this new area of research for the institute, aligned with HMRI’s mission to examine the heart-brain connection. Her work helps scientists better understand the mechanics of heart failure and brain aging.

Signal pathways are the underlying communication system within a cell, allowing it to receive, process and transmit signals within itself and with the environment around it. Dr. Purcell is interested in pathways that become altered with brain aging or cardiovascular injury. Her team is investigating two types of proteins called PHLPP1 and PHLPP2, which are important for cell stability and metabolic regulation. When both proteins are removed, they disrupt the pathways important for cell survival and can cause cancerous tumors to grow. However, the removal of only PHLPP1 may have a therapeutic effect. They are working to understand the cellular targets of the PHLPP proteins in the heart and brain, which can lead to the development of therapeutic strategies to treat these conditions.
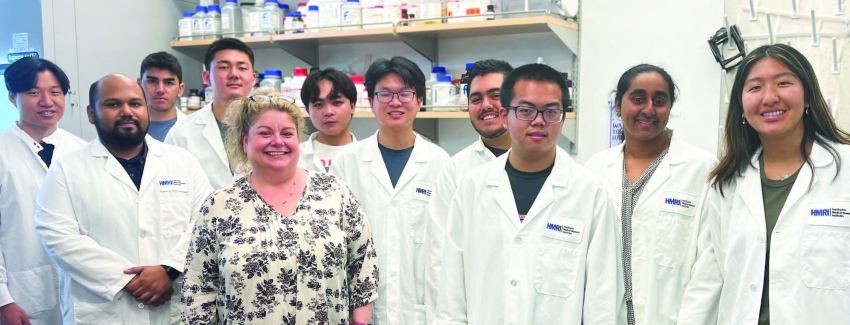
High School STEM Program Launches
In addition to a tradition of scientific discovery, HMRI has a long history of providing research opportunities for postdoctoral scientists and graduate and undergraduate students. In 2021, HMRI appointed Nicole H. Purcell, PhD, as the institutes’ scientific director of Education Programs. Dr. Purcell expanded the program to add laboratory-based opportunities through a new Science, Technology, Engineering, and Mathematics (STEM) Program for Pasadena high school students. Since her arrival, Dr. Purcell has worked to develop more structured educational experiences for students and postdoctoral fellows. Her vision is for HMRI to be a recognized destination of choice for the next generation of scientists.

Scaling Scientific Discovery and Innovation
The Analytical Biochemistry Core Laboratory (ABC) was established in January 2023 to foster growth and scalability at HMRI, enhancing focused research and innovation. This shared resource supports researchers with analytical methodologies using advanced detection systems for the identification, characterization, and quantification of compounds and their interactions. As a well-equipped testing facility with state-of-the-art instrumentation, the ABC lab uses electrochemiluminescence platforms (MSD), chromatography systems, spectrophotometry analyzers, and sample preparation equipment to execute various techniques in biological and synthetic matrices.
Immunology Provides New Insights into the Heart-Brain Connection
HMRI strategically added the Neuro-Cardio-Immunology Lab in 2023, led by Abdala Elkhal, PhD, assistant professor of Immunology. This highly synergistic and complementary area of research expands the breadth of HMRI’s scientific discovery into the vital connection between the heart and brain. Immunology has implications for HMRI’s existing programs that research neurodevelopment, neurodegenerative diseases, cardiovascular pathogenesis, and cardiovascular molecular mechanisms. Dr. Elkhal’s research primarily focuses on the role of the naturally occurring coenzyme Nicotinamide adenine dinucleotide (NAD+), which is present in all living organisms and central to energy metabolism. A decade ago, he made a ground-breaking observation in preclinical trials – NAD+ exhibited significant potential as a therapy for individuals suffering from autoimmune disorders, bacterial infections, and organ transplantation.

While serving on the faculty at Harvard, Dr. Elkhal discovered that administering NAD+ provided protection against septic shock induced by bacteria like E. coli. Additionally, NAD+ not only impeded the progression of the autoimmune disease multiple sclerosis but also reversed its advance. At HMRI, Dr. Elkhal collaborated with Dr. Vasudevan. In their preclinical models, NAD+ repaired flawed blood vessel formation in the embryonic forebrain, preventing abnormal behavioral symptoms after birth. Together with Dr. Kloner, Dr. Elkhal is exploring the potential of NAD+ as a therapeutic intervention for patients recovering from heart attacks and to minimize excessive bleeding following major injuries.

Princeton IV: PDE-5 Inhibitors and Cardiac Health Symposium
Twenty-five years after Viagra first hit the market, a group of experts from across the country examined the link between erectile dysfunction (ED) and heart health. This group of interdisciplinary scientists convened “Princeton IV: PDE-5 Inhibitors and Cardiac Health Symposium” in March 2023, held at HMRI. This expanded upon Princeton III, held over a decade ago. Scientists determined that PDE-5 inhibitors are still safe for the cardiovascular system and made additional clinical recommendations for men who present with ED. Dr. Kloner, also a professor of medicine at Keck School of Medicine of the University of Southern California (USC), was Princeton IV’s principal investigator. He led the group with co-chair Raymond Rosen, PhD of the University of California San Francisco, steering committee members Arthur L. Burnett, MD, MBA of Johns Hopkins, and Martin M. Miner, MD of Brown University.
Advancing Research on Alzheimer’s Disease
The Brain Aging Study continues to grow, positively impacting society and aging populations. Dr. Astrid Suchy-Dicey, who joined HMRI in October 2023, led the study for two years through July of 2025. Dedicated to unraveling health disparities in neurodegenerative diseases, her research focuses on enhancing methodology for analyzing and interpreting data related to imaging, biomarkers, cognitive testing, and social determinants pertaining to Alzheimer’s and vascular diseases, especially in American Indians, Alaska Natives, and other marginalized populations. She is committed to risk and resilience factors as she leads multiple large, landmark population-based studies on Alzheimer’s disease and related dementias.
The future of HMRI’s Brain Aging Study, now led by Dr. Kloner, will advance research on Alzheimer’s disease. Researchers will continue to expand recruitment in Pasadena and surrounding communities.

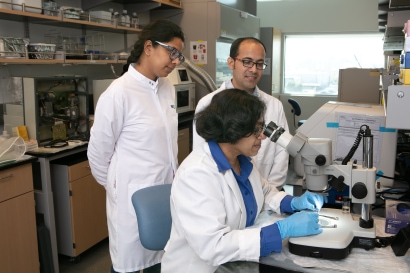
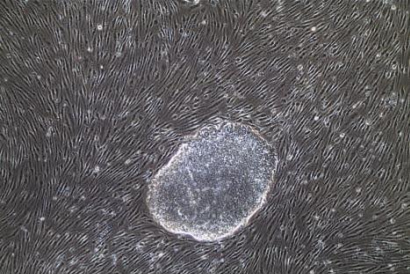
HMRI Launches Translational Pluripotent Stem Cell Program
The Angiogenesis and Brain Development Laboratory (ABDL), led by Dr. Anju Vasudevan, began pioneering research using translational pluripotent stem cells in 2024. While the field of induced pluripotent stem cell (iPS)-based psychiatric research is still developing, it has the potential to shed light on the “black box” of human prenatal brain development. The ABDL team can apply knowledge from the control of human embryonic forebrain-like endothelial cells to study intrinsic defects in endothelial cells from patient-derived iPSs of any psychiatric disorder. They expect to identify novel endothelial-associated cellular and molecular phenomena that underlie disease pathogenesis, opening new avenues for the diagnosis and treatment of mental illnesses.
